Training
To be board-certified in the field of Pain Medicine, a doctor completes a residency in a specialty, such as Anesthesiology, Physical Medicine and Rehabilitation, or Neurology. Primary board certification in the field of residency training can then be obtained. In order to be board-certified in Pain Medicine, an additional 1-2 years of sub-specialized training must be completed through a fellowship program associated with an academic institution or university. Only after completing a residency, fellowship, and receiving a board certification in the primary field is a physician permitted to seek board certification in Pain Medicine as a secondary, or sub-specialty, certification. Board certification in any field doesn’t necessarily guarantee a certain level of care, but it does indicate that the physician has repeatedly demonstrated a high competency and proficiency standard that is substantiated and backed by the American Board of Medical Specialties.
Knowledge
Board-certified Pain Medicine Specialists have undergone rigorous training, specific to addressing the myriad of conditions that cause pain, in both acute and chronic settings. This knowledge includes the physiological mechanisms that initiate or perpetuate pain signals in the body, the mechanisms by which medications can intervene on these processes, and the impact of pain on the individual by addressing the psychosocial impairment that often accompanies painful conditions.
Skillset
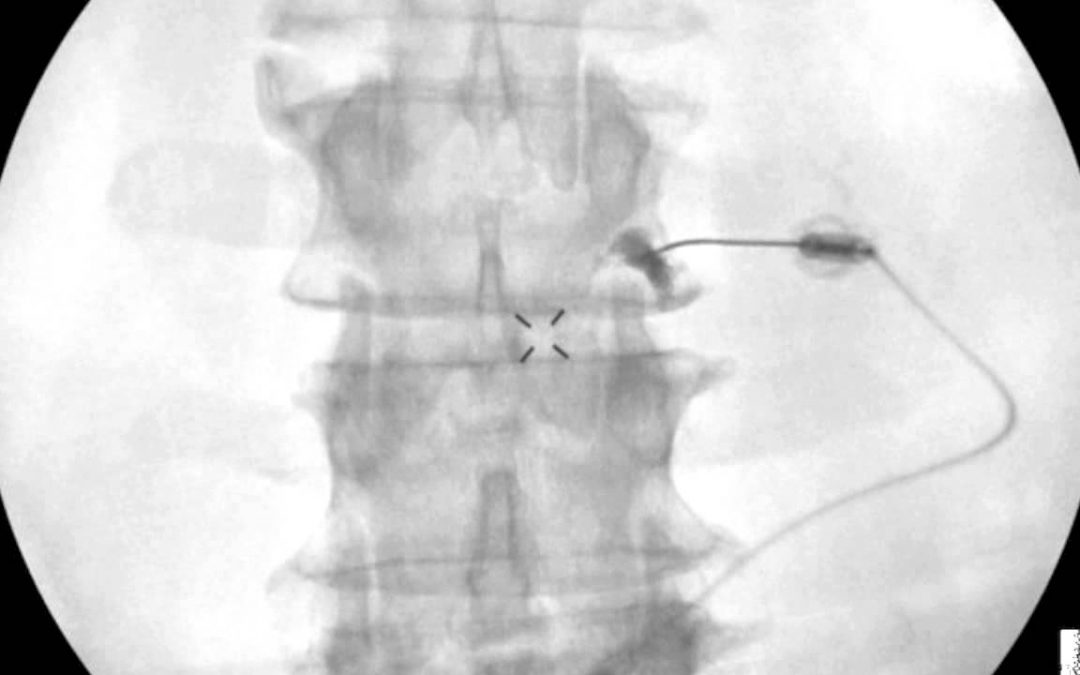
In addition to the qualifications listed above, an interventional Pain Medicine Specialist also has uniquely honed procedure skills. The vast majority of interventions are done with some form of image guidance, either X-ray or ultrasound. This helps to ensure the procedure is done in the safest manner, maximizes the potential therapeutic benefits, and minimizes pain and trauma from the procedure itself. The procedure will vary depending on the condition being treated, but may include an ultrasound-guided injection of a small peripheral nerve near the ankle to control foot pain, an X-ray-guided epidural injection in the lumbar spine to control back and leg pain, or a radiofrequency ablation of a spinal spinal joint to relieve arthritic back or neck pain. In any procedure, specialist-level knowledge and understanding of neuro and skeletal anatomy is necessary to achieve the best outcomes.
Responsibility
Given the extensive training in physiology, pathology, anatomy, and pharmacology of painful conditions, Pain Medicine Specialists are uniquely positioned to help address the country’s opioid epidemic. It is incumbent to explore alternative options to opioids for pain control whenever possible. And when other alternatives have been exhausted, to help guide opioid treatment.